Reference: UK Resuscitation Council ‘Newborn resuscitation and support of transition of infants at birth Guidelines’ 2021
Please note OSCEstop content is for educational purposes only and not intended to inform clinical practice. OSCEstop and authors take no responsibility for errors or the use of any information displayed.
Preparation
- Before birth: gather equipment, confirm gestation, foetal distress, meconium
- Cord should be clamped after at least 1 minute if possible/immediate resuscitation not required (if not possible, cord milking is an option in babies >28 weeks gestation)
- Keep baby warm (maintain temperature between 36.5-37.5°C)
- >32 weeks: dry baby; cover head and body with warm towel; use radiant warmer if baby needs support or when resuscitation (if not, skin-to-skin with mother)
- ≤ 32 weeks: completely cover with polyethylene wrapping (apart from face) without drying; use radiant warmer
- Start timer
Initial assessment
- Tone and colour (muscle tone, pallor)
- Breathing (established/crying, pattern, gasping/grunting)
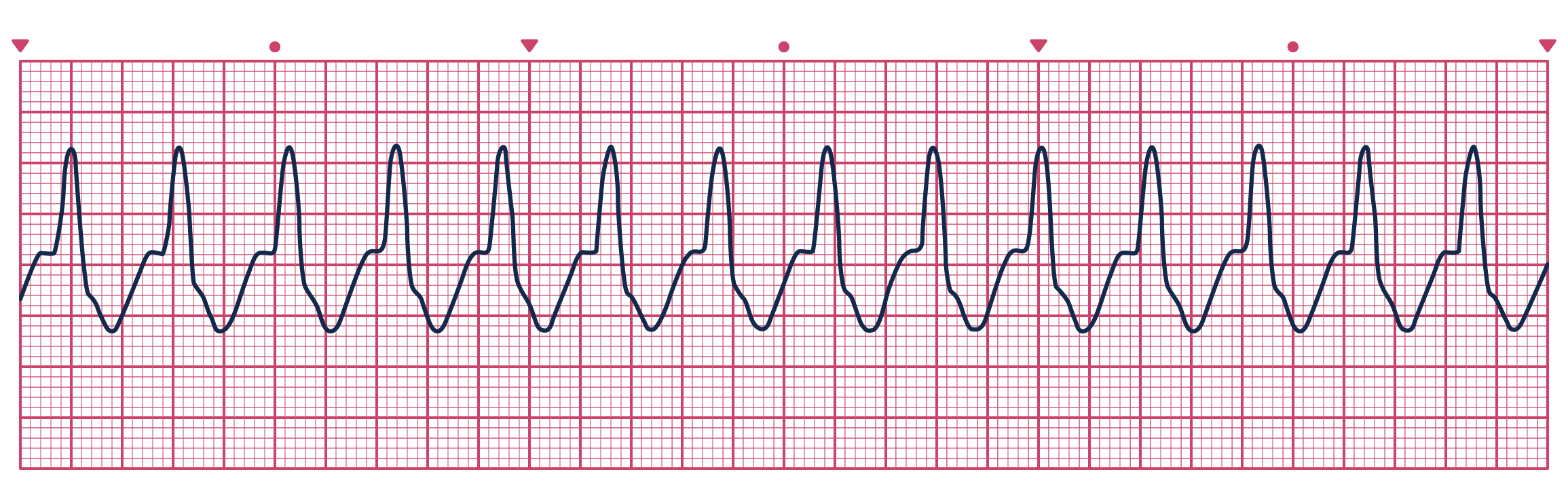
- Heart rate (>100bpm satisfactory; <60bpm critical) – key observation (assess using oximeter on right hand/wrist)
If heart rate <100bpm or breathing abnormal:
-
- Establish and maintain open airway
-
- Give 5 inflation breaths via bag and mask, maintaining the inflation pressure for 2-3 seconds (watch for adequate chest expansion)
-
- Oxygenation
-
- ≥32 weeks gestation - 21% oxygen (air)
-
- 28-32 weeks – 21-30% oxygen
-
- NB. if <32 weeks, titrate oxygen to aim sats >80% at 5 mins.
-
- If chest not expanding adequately:
-
- Try jaw-thrust (2-person technique preferred) ± Oropharyngeal airway and suction
-
- Check mask size, position and seal
-
- Give 5 further inflation breaths
-
- If still not expanding adequately, check for obstructing foreign matter; consider tracheal intubation or laryngeal mask
When 5 inflation breaths performed with adequate chest expansion:
- Re-assess (tone and colour; breathing; heart rate)
↘ If heart rate <60bpm or absent:
-
- Start chest compressions (3:1 compressions:breaths at about 15 cycles every 30 seconds)
-
- 100% inspired oxygen initially then titrate
-
- Re-evaluate the response every 30 seconds
-
- If heart rate still <60bpm
↘ If heart rate >60bpm:
- Breathing not established →
- Continue ventilations until breathing established, at around 30 breaths/min with an inflation time of around 1 second
- Re-assess every 30 seconds
- Breathing established → hand back to mother but monitor closely
Ventilation technique (after 5 inflation breaths)
- Ensure head is in neutral position
- Inflation time of around 1 second
- Ventilation rate of around 30 breaths/min
- Watch for chest movement
- Tracheal intubation may be required for prolonged resuscitation, severe meconium aspiration or diaphragmatic hernia
- If no chest movement
- Try jaw-thrust or Guedel airway
- Look for airway obstruction – consider suction
- May need higher positive pressure (e.g. if lung hypoplasia, diaphragmatic hernia)
- If intubated – consider position of tracheal tube
- Target saturations (attach monitor to right hand/wrist)
- 1-5minutes: 70-80%
- 5-10 minutes: 80-85%
- >10 minutes: 85-95%
- If low, increase oxygen in increments of 20%.
Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions
Compression technique
- Technique
- From caudal end, grasp both your hands around their chest
- Place one thumb on top of the other over the sternum just below imaginary line between nipples
- Compress the chest diameter by one third
- 3:1 compression:breaths ratio at around 15 cycles every 30 seconds
- Another person should perform ventilations – if you are alone, use 2 fingers to perform compressions and hold the mask in place with your other hand
- Re-assess every 30 seconds
Drugs
Please note OSCEstop content is for educational purposes only and not intended to inform clinical practice. OSCEstop and authors take no responsibility for errors or the use of any information displayed.
Should be given via umbilical venous access (usually), intravenously, or intraosseously. Estimate birth weight to calculate doses. In usual order:
- Adrenaline 1:10,000 0.2ml/kg (20micrograms/kg) IV, can be repeated every 3-5 minutes if heart rate remains <60bpm
- Glucose 10% 2.5ml/kg IV in prolonged resuscitation
- Sodium bicarbonate 4.2% 2-4ml/kg IV in prolonged unresponsive resuscitation
- 10ml/kg fluid bolus (0.9% saline) IV or O Rh-negative blood if suspected blood loss or shock unresponsive to other resuscitative measures