Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions
Ask patient to sit forwards:
Ask patient to sit back:
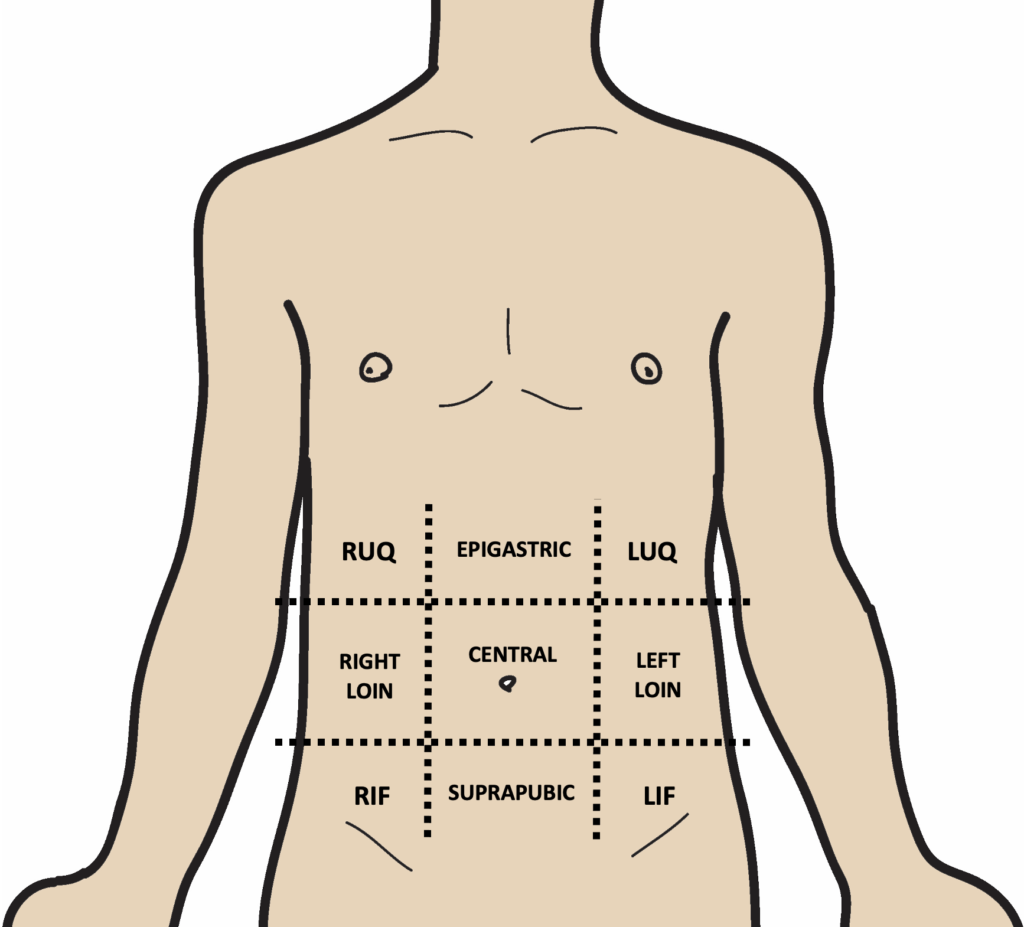
Closely look at the patient’s abdomen for:
Superficial palpation


Crouch to patient’s level and gently roll fingers of your right hand over each of the nine regions while watching the patient’s face
Check for: tenderness, guarding (peritonitis), rebound tenderness (peritonitis)
Deep palpation


Palpate again but deeply using both hands – the upper hand to exert pressure, the lower hand to feel. (You can be standing for this.)
Check for: masses, deep tenderness and, if relevant, Rovsing’s sign (appendicitis) and Murphy’s sign (cholecystitis).
Liver palpation


Ask the patient to breathe in and out deeply.
Using the radial border of the right hand, palpate in increments from the RIF to the right costal margin – push in on each inspiration.
Hepatomegaly may be caused by: metastasis/hepatocellular carcinoma, hepatitis, RVF, leukaemia/lymphoma, fatty liver, alcoholic liver disease.
Spleen palpation


Palpate the spleen in the same way as the liver, but diagonally from the RIF to the left costal margin. The spleen can be felt better if patient rolls onto their right side with tucked legs.
Splenomegaly may be caused by: lymphoma/leukaemia, myelofibrosis, myeloproliferative disorders, portal hypertension, extravascular haemolysis, malaria/EBV.
Kidney palpation


Place one hand anteriorly and one posteriorly in the patient’s loin.
Ask patient to expire as you press up into renal angle with your posterior hand and press down with your anterior hand.
As patient breathes in, you may feel the kidney between your hands.
Ballot the kidney by flexing the MCP joints of your posterior hand. Do flick, flick, stop and then repeat as necessary.
Aorta palpation


Press down with finger tips (one hand each side) in the horizontal plane midway between the umbilicus and xiphoid process, starting laterally and moving medially.
The ulnar borders of your hands should be parallel with the costal margins.
Pulsatile mass, i.e. upward movement, can be normal; expansile mass, i.e. outward movement, suggests AAA.
How to… Differentiate between the spleen and left kidney
Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions
Name five causes of abdominal distension


Oops! This section is restricted to members. Click here to signup!
What clinical examination features would suggest decompensation of chronic liver disease?


Oops! This section is restricted to members. Click here to signup!
In what circumstances might you be able to palpate a kidney?


Oops! This section is restricted to members. Click here to signup!
What are the causes of hepatosplenomegaly?


Oops! This section is restricted to members. Click here to signup!
What are the complications of stoma formation?


What are the most common pathologies requiring a renal transplant?


Oops! This section is restricted to members. Click here to signup!
Name, describe and list the indications for each of the the three types of colostomy?


Oops! This section is restricted to members. Click here to signup!
How is chronic liver disease managed?


Picture references


Clubbing: 2009 Desherinka, licensed under the Creative Commons Attribution-Share Alike 4.0 International (https://creativecommons.org/licenses/by-sa/4.0/), 3.0 Unported (https://creativecommons.org/licenses/by-sa/3.0/deed.en), 2.5 Generic (https://creativecommons.org/licenses/by-sa/2.5/deed.en), 2.0 Generic (https://creativecommons.org/licenses/by-sa/2.0/deed.en) and 1.0 Generic license (https://creativecommons.org/licenses/by-sa/1.0/deed.en) and GNU Free Documentation licence 1.2 (https://commons.wikimedia.org/wiki/Commons:GNU_Free_Documentation_License,_version_1.2). Sourced from: https://en.wikipedia.org/wiki/Nail_clubbing#/media/File:Dedos_con_acropaquia.jpg
Dupuytren’s contracture: 2010 James Heilman, MD, Creative Commons Attribution-Share Alike 3.0 Unported license (https://creativecommons.org/licenses/by-sa/3.0/deed.en). Sourced from: https://commons.wikimedia.org/wiki/File:Dupuytren%27s2010.JPG
Xanthelasma: 2005 Klaus D. Peter; licensed under the Creative Commons 3.0 Germany licence (https://creativecommons.org/licenses/by/3.0/de/deed.en). Sourced from: https://commons.wikimedia.org/wiki/File:Xanthelasma.jpg
Glossitis: 2011. Grook Da Oger. Licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license (https://creativecommons.org/licenses/by-sa/3.0/deed.en). Sourced from: https://commons.wikimedia.org/wiki/File:Glossite.jpg
Spider naevi: 2018. James Heilman, MD. Licensed under the Creative Commons Attribution-Share Alike 4.0 International license (https://creativecommons.org/licenses/by-sa/4.0/deed.en). Sourced from: https://commons.wikimedia.org/wiki/File:SpiderAngioma.jpg
Gynaecomastia: 2021. ProloSozz. Licensed under the Creative Commons Attribution-Share Alike 4.0 International license (https://creativecommons.org/licenses/by-sa/4.0/deed.en). Sourced from: https://commons.wikimedia.org/wiki/File:Gynaecomastia.jpeg
Ascites (second photo): 2011. James Heilman, MD. Licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license (https://creativecommons.org/licenses/by-sa/3.0/deed.en). Sourced from: https://commons.wikimedia.org/wiki/File:Hepaticfailure.jpg
Pitting oedema: James Heilman, licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license (https://creativecommons.org/licenses/by-sa/3.0/deed.en). Sourced from: https://en.m.wikipedia.org/wiki/File:Combinpedal.jpg
Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions
[…] https://oscestop.education/clinical-examination/abdominal-examination/ […]