In order to understand which antibiotics patients require, it is necessary to know which infective organisms you needs to cover (outlined on this page) and which antibiotics cover which organisms (outlined here).
Community-acquired pneumonia
If immunocompromised (e.g. malnourished, alcoholic, diabetic, on long-term steroids), also: Staphylococcus aureus, coliforms, TB
If severely immunosuppressed (e.g. HIV with CD4 <200, transplant recipient), also: Pneumocystis carinii, Cryptococcus, CMV, Varicella zoster virus, influenza, fungal infections
Hospital-acquired pneumonia
Colonising bacteria in chronic respiratory diseases
In cystic fibrosis, also: Burkholderia cepacia
Upper respiratory tract infections
Cavitating pneumonia
Intra-abdominal (including biliary)
Normal bowel flora:
Gastroenteritis/diarrhoea
Less common: Yersinia enterocolitica, Bacillus cereus, Staphylococcus aureus
If risk factors, also: Clostridium difficile, Vibrio cholerae, Salmonella typhi
If dysentery: Shigella, Vibrio cholerae, amoebiasis
Don’t forget viral, parasitic and non-infectious causes!
Skin/joints/bone
For wound/ulcer infections or severe/necrotising cellulitis, also: anaerobes
For burns, also: anaerobes, Pseudomonas
For post-surgical wounds, also: Gram negative bacilli (e.g. E. coli, Klebsiella, Pseudomonas), Enterococci, MRSA, CONS
NB: wound-colonising bacteria (i.e. bacteria present in exudate without necessarily causing infection) include: coliforms, Enterococcus, anaerobes
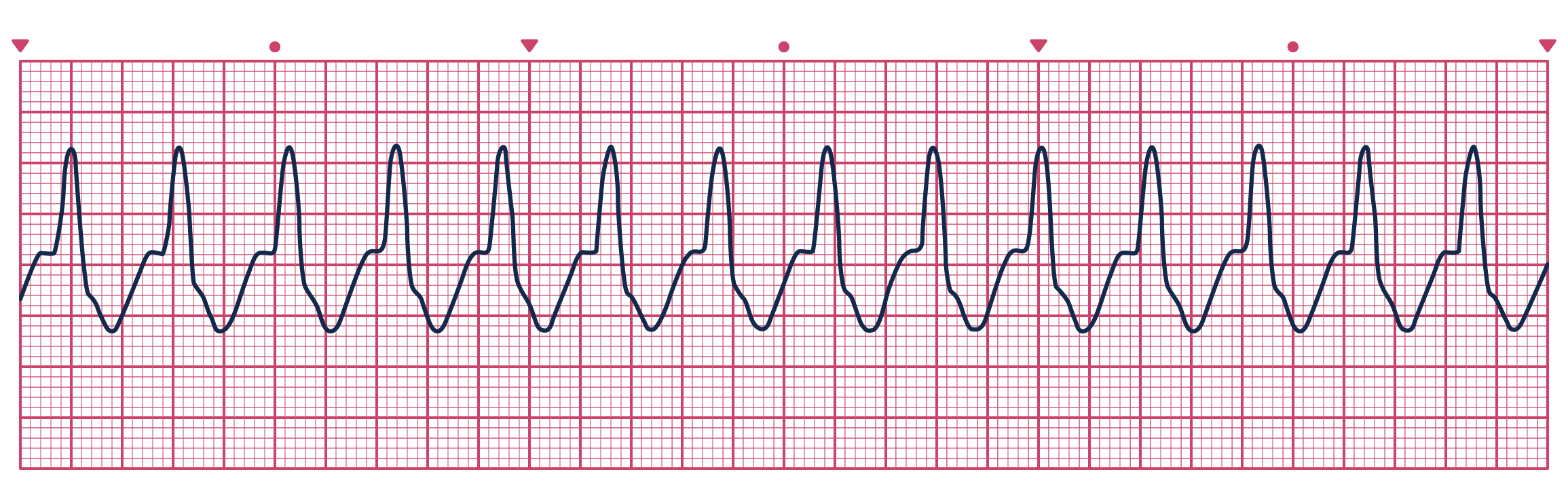
A patient presents to ED with chest pain and this trace. What would you do?
Interpretation management
Meningitis
If neonatal: group B Streptococcus, E. coli/coliforms, Listeria (rare)
Urine infections
Less common organisms (3) are associated with: catheters, hospitals, structural abnormalities and instrumentation
Infective endocarditis
Surgical prophylaxis
Sepsis of unknown origin
Want to find out how 99% of people passed their exams?
Here are some syndromes associated with group A streptococcus (Streptococcus pyogenes). Outline the cause, timeframe and clinical features of each.
Scarlet fever
Oops! This section is restricted to members. Click here to signup!
Streptococcal toxic shock syndrome
Oops! This section is restricted to members. Click here to signup!
Post-streptococcal glomerulonephritis
Oops! This section is restricted to members. Click here to signup!
Rheumatic fever
Oops! This section is restricted to members. Click here to signup!
Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions