Please note OSCEstop content is for educational purposes only and not intended to inform clinical practice. OSCEstop and authors take no responsibility for errors or the use of any information displayed.
NOTE: in paediatrics medication doses must be evenly spaced, so prescribe ‘hourly’ rather than TDS/QDS
Emergencies
You must know these:
- Cardiac arrest: DC shock 4J/kg biphasic, Adrenaline 1:10,000 IV 0.1ml/kg (10mcg/kg), Amiodarone 5mg/kg IV
- Anaphylaxis: Adrenaline 1:1000 IM <6 years 150mcg (0.15ml), 6-12 years 300mcg (0.3ml), >12 years 500mcg (0.5ml)
- Seizure: Lorazepam 0.1mg/kg IV (max 4mg; or, if no IV access, Diazepam 0.5mg/kg PR or Buccal midazolam 0.5mg/kg TOP)
- Sepsis: Ceftriaxone 80mg/kg IV
- Stridor: Adrenaline nebuliser 0.5ml/kg 1:1000 NEB (max 5ml)
- Hypoglycaemia: 10% dextrose 2.5ml/kg IV or Glucagon IM neonate 20mcg/kg, <25kg 500mcg, >25kg 1mg (if no IV access) or 0.3g/kg PO glucose gel or tablets
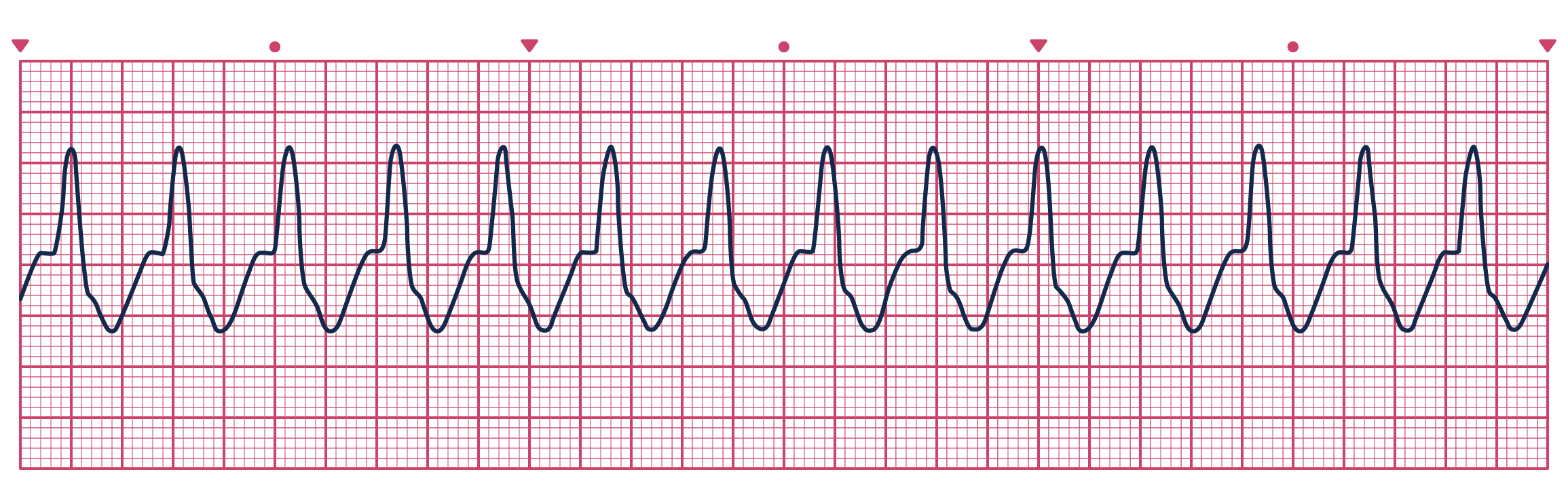
- SVT (without adverse signs): Adenosine 100mcg/kg IV (can be followed by repeated doses increasing by 50-100mcg/kg until terminated or maximum single dose 500mcg/kg)
- VT (without adverse signs): Amiodarone 5mg/kg IV over 30mins (maximum 300mg)
- Tachycardic arrhythmia (with adverse signs): Synchronised DC shock 1J/kg (can be followed by 2J/kg shocks)
- Bradycardia (due to increased vagal tone): Atropine 20mcg/kg IV (maximum 600mcg single dose)
Analgesia
- Paracetamol 20mg/kg PO loading dose then 15mg/kg 8-hourly <1 month or 6-hourly >1 month (max: 30mg/kg/d <1 month, 60mg/kg/d <3 months, 1g/dose >3 months)
- Morphine 0.2mg/kg PO or 0.1mg/kg IV
- Intranasal diamorphine 0.1mg/kg TOP
Fluid bolus
- Normal saline 20mg/kg IV (may given by 50ml syringes in infants)
Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions
Nausea/vomiting >2 years old
- Ondansetron 100mcg/kg IV (maximum 4mg)
Wheeze
- Salbutamol 10 puffs inhaler INH via spacer (or 2 puffs and increase by 2 puffs every 2mins depending on response – max 10 puffs)
- Salbutamol 2.5mg NEB PRN 4-6hourly (max 20mg)
- Ipratropium bromide 250micrograms NEB, PRN 4-6hourly (max 2mg)
- Prednisolone 1-2mg/kg PO OD (max 40mg)
Electrolyte replacement
Hypokalaemia
- Mild (>2.5mmol/L): Sando-K tablets (12mmol/tablet) or Kay-Cee-L liquid (1mmol/ml) 0.5-1mmol/kg PO BD x 3/7 (max 72mmol/day)
- Severe (<2.5mmol/L or symptomatic): Potassium chloride 1mmol/kg over 6-12 hours using ready-made solution of 20mmol potassium chloride in 500ml 0.9% saline or 0.9% saline/5% dextrose IV (max rate 0.2mmol/kg/h without ECG monitoring)
Hyperkalaemia
1. ECG and cardiac monitoring
2. Calcium gluconate 10% 0.5ml/kg IV (max 20ml) over 5-10 mins – can be used undiluted in emergencies
3. Actrapid insulin 0.1units/kg in 2ml/kg 25% dextrose IV over 30 mins
Hypocalcaemia
- Calcium gluconate 10% 0.5ml/kg IV (over 30mins, max 10ml) – should be diluted: 1ml 10% calcium gluconate to 4ml normal saline or 5% dextrose
Hypomagnesemia
- Mild (>0.5mmol/L): Magnesium glycerophosphate 4mmol tablets (can be divided to smaller doses) 0.2mmol/kg PO every 8 hours (max 8mmol/dose) x 3/7
- Severe (<0.5mmol/L or symptomatic): Magnesium sulphate 10% 0.5-1ml/kg (over 2 hours, max 20ml) – note 10ml of 10% = 1g = 4mmol
Hypophosphataemia
- Mild (>0.65mmol/L): Phosphate-Sandoz effervescent tablets (16.1mmol/tablet) 2-3mmol/kg PO daily in 2-4 divided doses x 3/7 (max 48mmol/day <5years, 97mmol/day >5years)
- Severe (<0.65mmol/L): Sodium glycerphosphate neonate 1mmol/kg, <2y 0.7mmol/kg, 2-8y 0.4mmol/kg, >25kg 10mmol (not per kg) IV over 12 hours – diluted to 0.02mmol/ml in normal saline e.g. 10mmol sodium glycerophosphate in 500ml normal saline