
おかげさまで開設25周年oscestop.education 創業祭
oscestop.education
マイストア
変更
お店で受け取る
(送料無料)
配送する
納期目安:
02月15日頃のお届け予定です。
決済方法が、クレジット、代金引換の場合に限ります。その他の決済方法の場合はこちらをご確認ください。
※土・日・祝日の注文の場合や在庫状況によって、商品のお届けにお時間をいただく場合がございます。
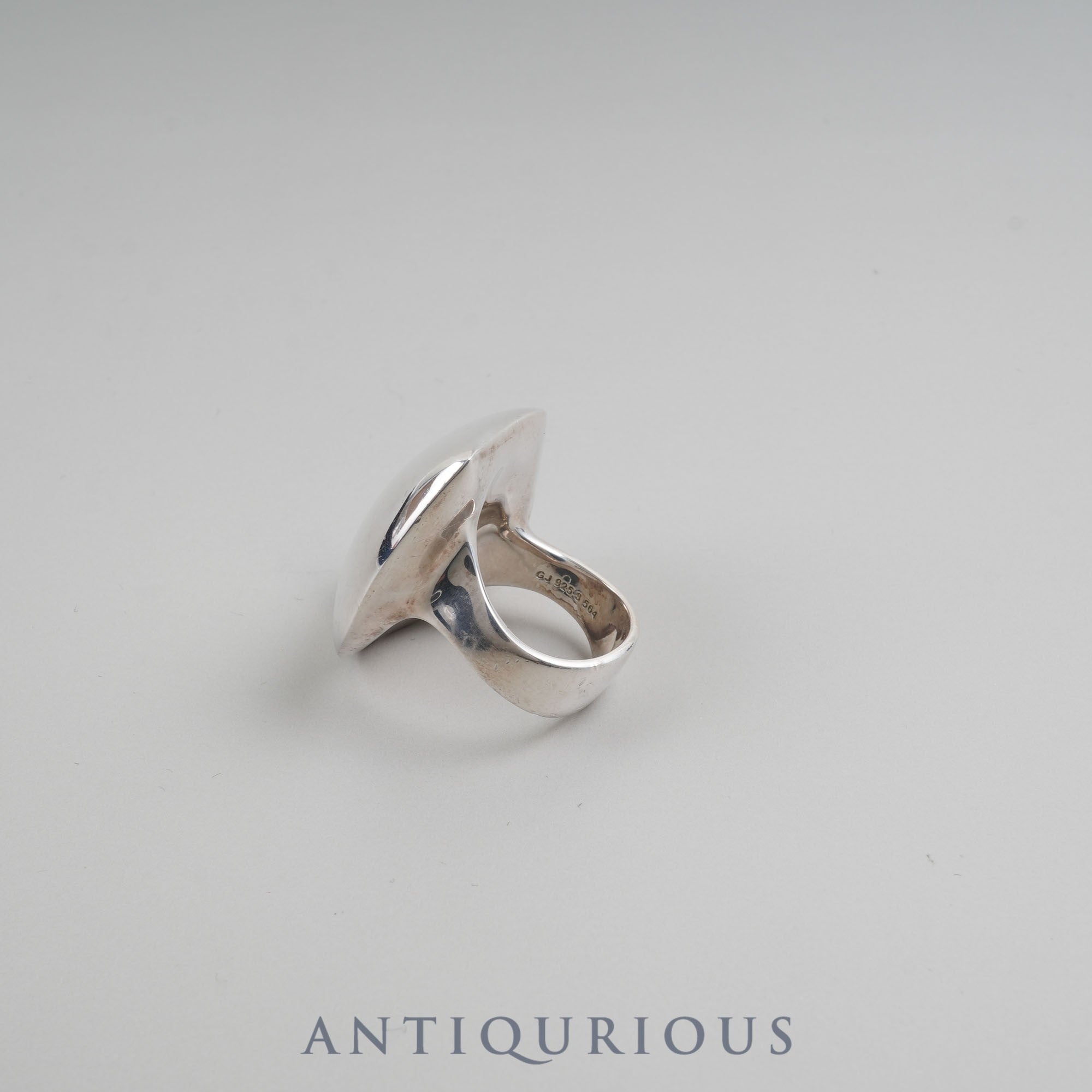
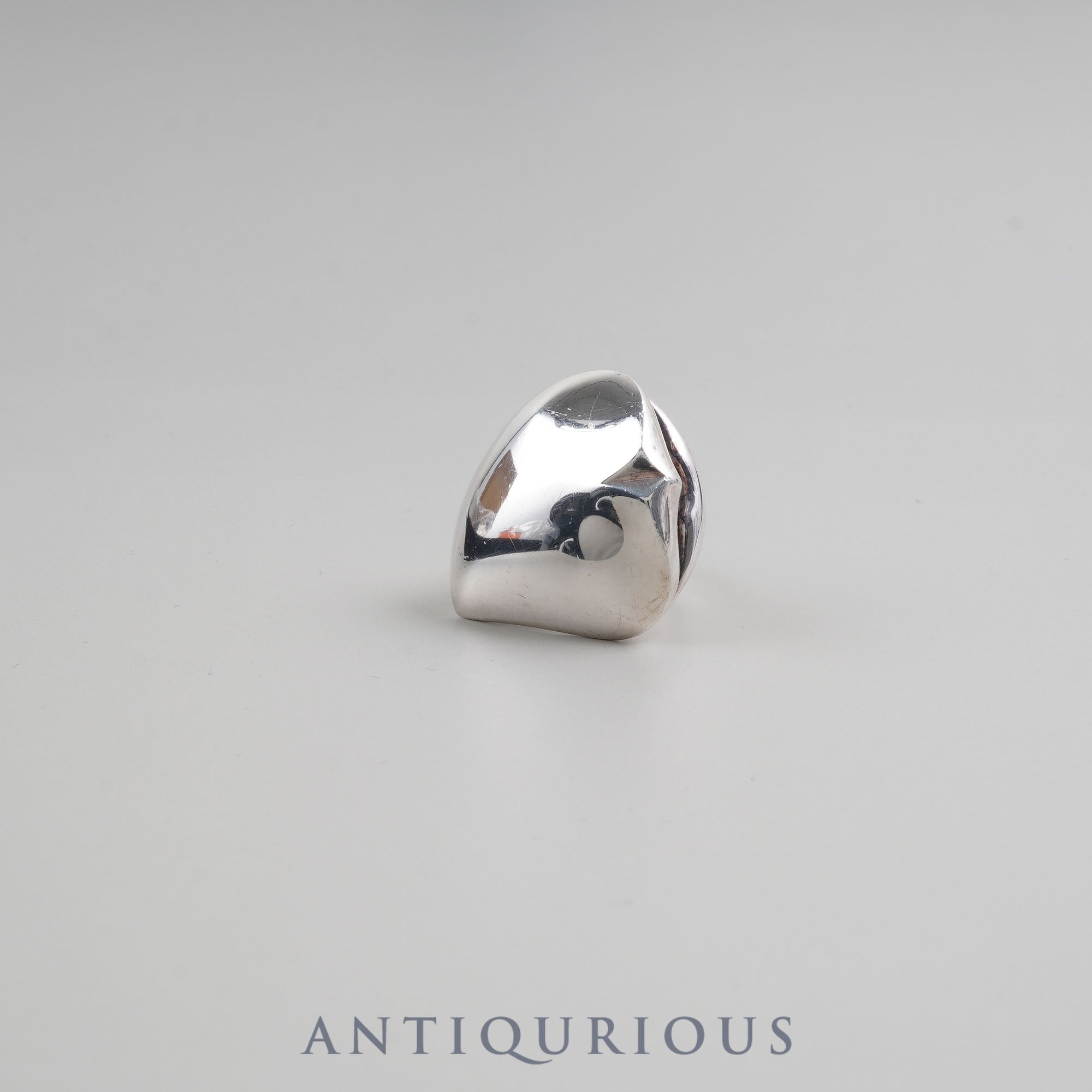
ジョージジェンセンsv925リング 22号 ジョージジェンセンsv925リング 22号 ジョージジェンセンsv925の詳細情報
ジョージジェンセンsv925リング 22号 ジョージジェンセンsv925
ジョージジェンセンsv925指輪
- 色: シルバー
- デザイン: 二重リング
- 素材: sv925
- 幅: 約7m m
神経質な方はご遠慮願います。
ご覧いただきありがとうございます。
商品の情報
| カテゴリー | ファッション > メンズ > アクセサリー |
|---|---|
| ブランド | Georg Jensen |
| 商品の状態 | やや傷や汚れあり,目につく傷や汚れがある |
ベストセラーランキングです
近くの売り場の商品
カスタマーレビュー
オススメ度 4.8点
現在、160件のレビューが投稿されています。























![【中古】展覧会の絵*組曲 [DVD]](https://tshop.r10s.jp/cometostore/cabinet/20240912-2/b00005ujko.jpg)



![[SRR-LV1261CS] 冷凍冷蔵庫 LVシリーズ パナソニック 業務用冷凍冷蔵機器 1室冷凍 803L(冷凍室186L、冷蔵室617L)](https://tshop.r10s.jp/sumai-rt/cabinet/common/car-deliverynote.jpg)