A discharge summary is an account of the major events of the hospital admission for the patient’s GP, so that they can take over the patient’s care.
Boost your productivity with an OSCEstop membership
📖 All OSCE Lerning
📟 OSCE stations
🔋 Qbank
💡 Conditions
NB: out-patient controlled drug prescriptions must be handwritten and must include patient name and address; drug, strength and formulation; dose and frequency. The total quantity must be spelled out as well as written numerically.
Who is responsible for following up outstanding results after the patient is discharged?
Oops! This section is restricted to members. Click here to signup!
Should the discharge summary be written in medical or lay language?
Oops! This section is restricted to members. Click here to signup!
Can you write a discharge summary for a patient if you were not involved in their care?
Oops! This section is restricted to members. Click here to signup!
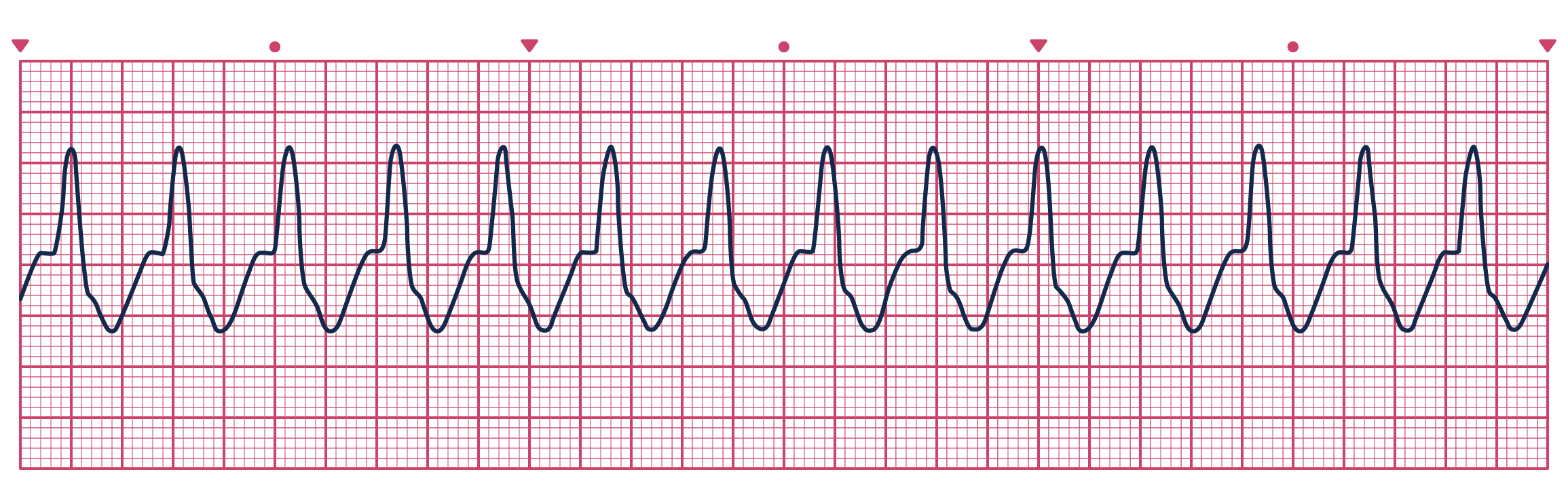
A patient presents to ED with chest pain and this trace. What would you do?
Interpretation management