Please note OSCEstop content is for educational purposes only and not intended to inform clinical practice. OSCEstop and authors take no responsibility for errors or the use of any information displayed.
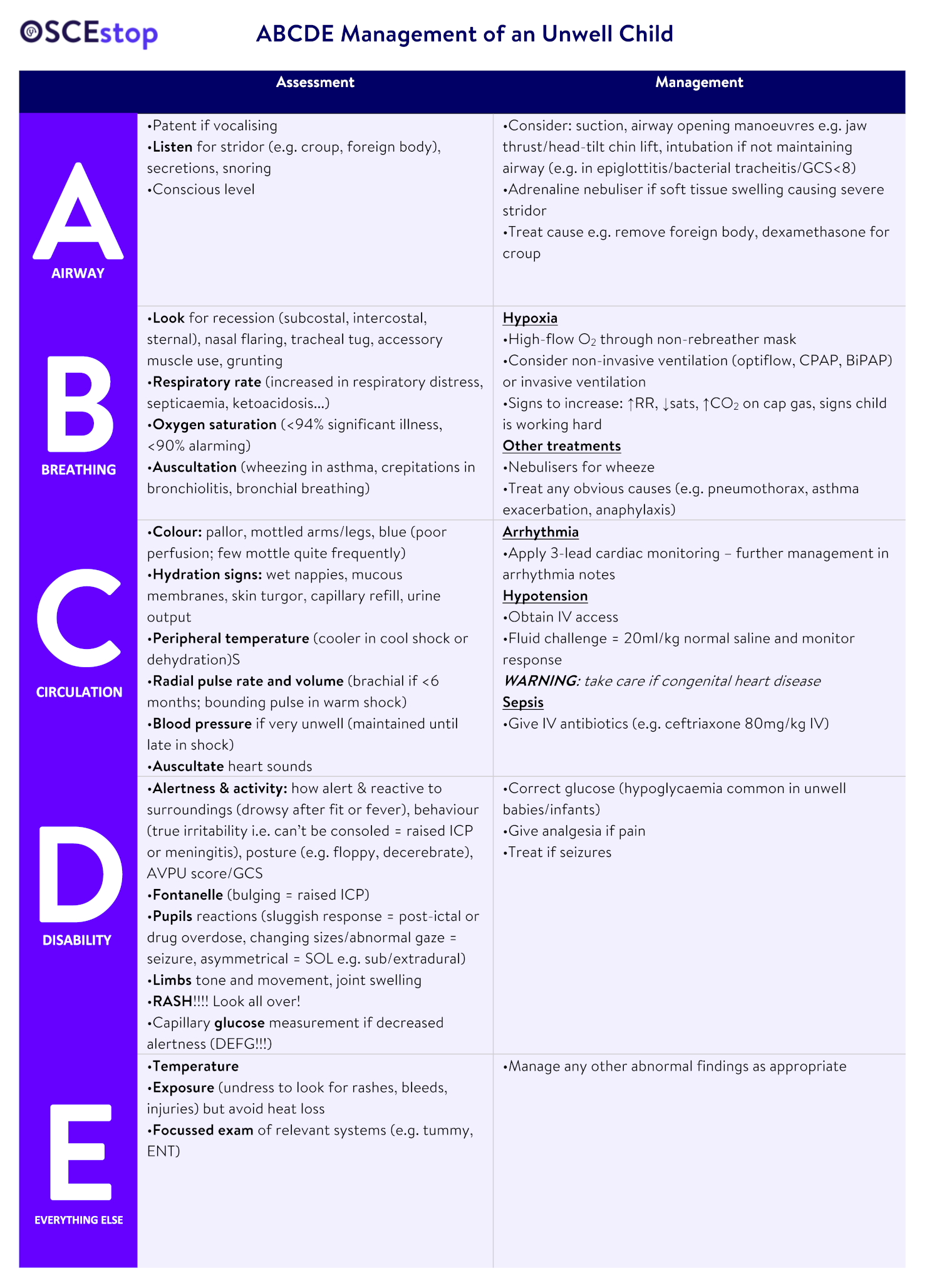
Note: Only move to the next letter when the one before has been treated, and keep re-assessing ABCDE from the start as necessary
| NORMAL | <1 year | 1-2 years | 2-5 years | 5-12 years | >12 years |
| Resp rate | 30-40 | 25-35 | 25-30 | 20-25 | 15-20 |
| Heart rate | 110-160 | 100-150 | 95-140 | 80-120 | 60-100 |
| Amber flags | Red flags | |
| A | Stridor | |
| B | Nasal flaring, tachypnoea, sats <95% | Respiratory distress (RR>60) |
| C | Pallor, tachycardia, reduced capillary refill, reduced UO, dry mucus membranes | Pale/mottled/blue, reduced skin turgor |
| D | Reduced activity, not responding normally to social cues | Unresponsive/won’t stay awake, non-blanching rash/neck stiffness, seizures |
| E | Rigors, fever in 3-6month old | Fever in <3month old |
Want to find out how 99% of people passed their exams?
You review a 2 year old in the emergency department. Her parents have brought her due to noisy breathing. On examination you hear stridor and notice subcostal recession. Observations are taken: respiratory rate 40, saturations 92% air, HR 160, temperature 39.2.
What is the differential diagnosis for stridor?


Oops! This section is restricted to members. Click here to signup!
You suspect the child has croup. What are the other signs of croup?


Oops! This section is restricted to members. Click here to signup!
What is the likely cause of the infection?


Oops! This section is restricted to members. Click here to signup!
You start an A-E assessment and are concerned about the airway. What would you do to manage this?


Oops! This section is restricted to members. Click here to signup!
Later in you shift you are called to the emergency department resus area. You are asked to review a 2 month old boy who is drowsy. The nurse has taken some observations, which show respiratory rate 40, heart rate 180, saturations 91% air, temperature 39.9. He is only responsive to pain on the AVPU scale. On examination he has dry mucus membranes and won’t stay awake. You undress him and notice he is mottled with a non-blanching rash.
What are the causes for a non-blanching rash?


Oops! This section is restricted to members. Click here to signup!
Which red and amber flags have you noticed?


Oops! This section is restricted to members. Click here to signup!
What diagnosis are you most concerned about?


Oops! This section is restricted to members. Click here to signup!
Which interventions would you include in each part of your A-E assessment?


Oops! This section is restricted to members. Click here to signup!
You are called to see a 13 year old on the paediatric assessment unit, referred in by their GP for an undifferentiated febrile illness. She has just returned from a 3 week holiday back to Nigeria, where she was born. The nurse has already done the observations and they show: respiratory rate 20, heart rate 140, oxygen saturations 99% air, temperature 40.1. On examination she is drowsy (alert to voice only). She looks dehydrated with dry mucus membranes and reduced skin turgor. There are no other focal examination findings and the chest is clear and abdomen soft and non-tender.
Which are the main parts of the A-E assessment you are concerned about? How would you manage them?


Oops! This section is restricted to members. Click here to signup!
Glucose is checked and is 2.1mmol/L. How would you manage this?


Oops! This section is restricted to members. Click here to signup!
Which investigations would you request?


Oops! This section is restricted to members. Click here to signup!
The lab calls to say the malaria test has come back positive. It looks like P. falciparum with a parasitaemia of 4%. What additional treatment would you give?


Oops! This section is restricted to members. Click here to signup!
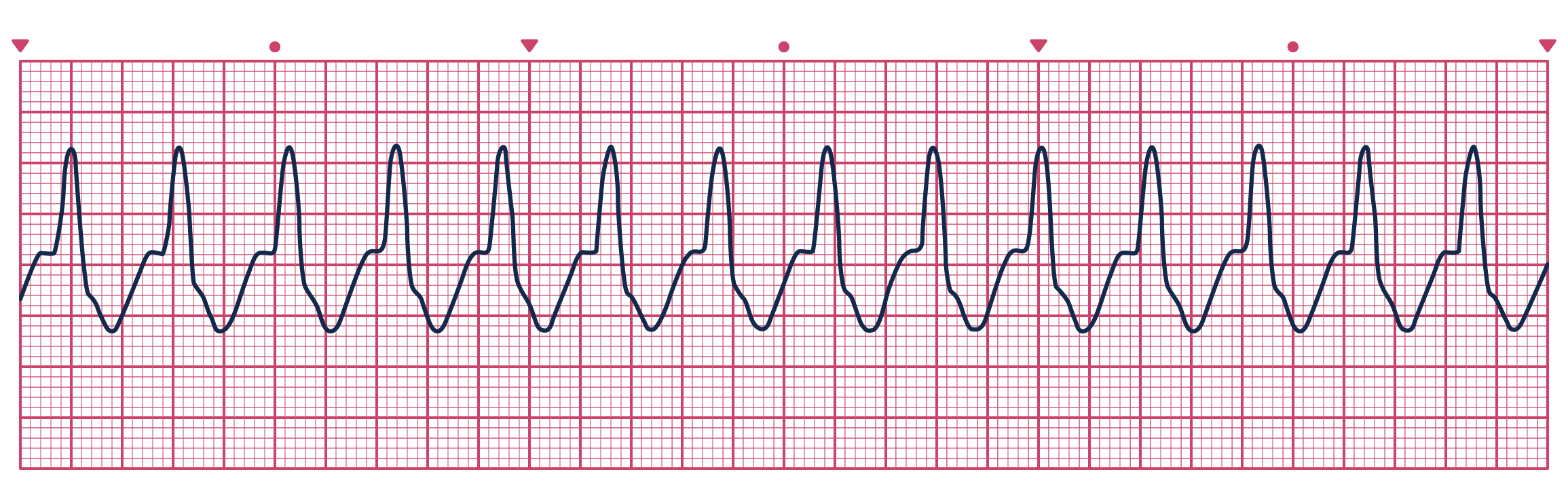
A patient presents to ED with chest pain and this trace. What would you do?
Interpretation management
Comments are closed for this post.